Orthopaedic Expert Care You Can Trust

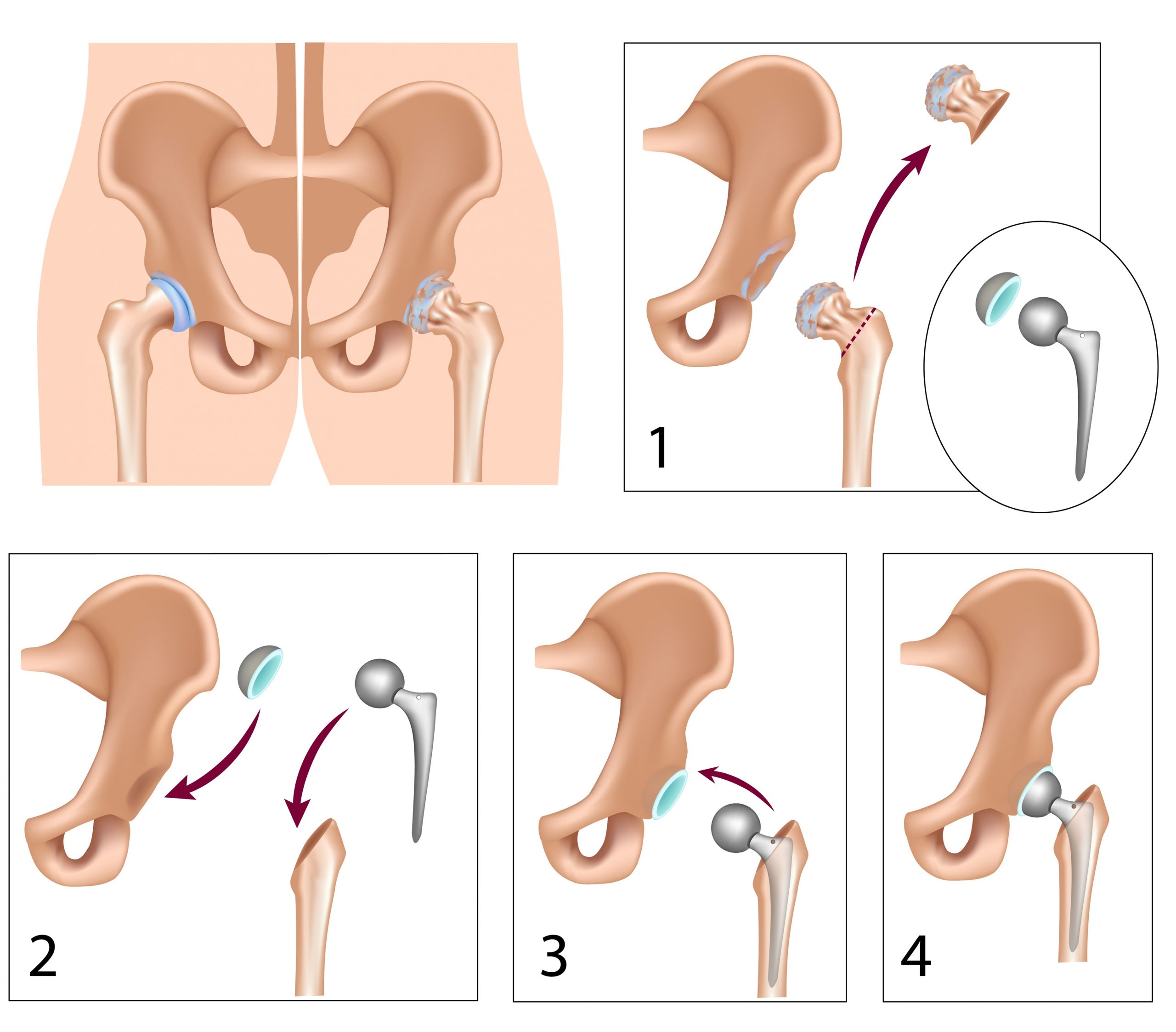
In this surgery (also called total hip arthroplasty), the worn out parts of the hip (the ball and the socket) are removed and replaced with artificial ones.
In the right patient this is one of the most successful operations known to man. In the UK, every patient that has a hip or knee replacement has their details entered in the National Joint Registry (NJR) and to date we have over 3 million entries. This is the largest database in the world and from this we can conclusively say that the success rates are 90-95%.
Why is it performed?
The most common reason for replacing a patient’s hip is because of significant arthritis in the joint. Hip replacement surgery can relieve pain and increase mobility, ultimately leading to a better quality of life. There are a number of reasons why arthritis can occur in the joint:
- Primary (or Osteoarthritis) in which there is no known cause and this can run in the family
- Rheumatoid arthritis (this is an a inflammatory type) which can affect multiple joints
- Untreated dysplasia of the hip (where the socket has not fully formed)
- Femoroacetabular impingement (FAI), where there is excess bone which keeps impacting on the rim of your socket, causing cartilage to tear
Hip replacement is also performed when patients have broken their hip (hip fracture). Whilst this most commonly occurs in older adults, I also see this injury in younger patients. This can be a result of stress fracture, when athletes have been training very hard and increased the intensity over a short period of time. Most of the time, an operation is not required, and more often than not the fracture can be fixed rather than the joint being replaced.
What does it involve?
Once a shared decision has been made to undergo a hip replacement, specific instructions will be provided on how to prepare for surgery and what to expect along the whole journey. You will be seen in a pre-operative nurse-led assessment clinic to determine your fitness for surgery. Following this, my PA will call you to look at convenient dates for surgery. As a result of minimally invasive surgery and the enhanced recovery protocols I use, patients stay in hospital for 2-3 days. Usually, patients are discharged on 2 crutches and then progress to one over the following 2 weeks. When they are seen at the 6 week follow-up period, they are frequently off crutches.
When can I drive and how long do I need to take off work?
Most people return to driving around the six week mark. Once again, due to the enhanced recovery program and minimally invasive techniques I use, I advise my patients to return to driving as soon as they can do an emergency stop. This can be around 3 to 4 weeks following surgery.
Return to work is that little more difficult to answer. This largely depends on the nature of your work. Often return to work correlates with when the patients can drive. Most patients take a minimum of six weeks off.
What are the risks of the operation?
All surgery carries risks. The main risks regarding this particular operation include:
Infection
This may be superficial or deep. Superficial infections are usually treated with antibiotics. Deep infections may require further surgery to eradicate the infection. A deep infection can be a life changing event but fortunately, this is a rare occurrence, and my infection rates are below the national average.
I regularly consult with my microbiologist to give the best possible antibiotics to prevent this complication from occurring. Keeping the surgical time to a minimum also helps prevent infection. I perform the surgery in a special laminar flow (ultra clean) operating theatre to further lower the risk of infection.
Blood clots
A blood clot in the leg is called a deep vein thrombosis (DVT). This can occur in either leg following surgery. A pulmonary embolism (PE) is when the clot migrates to the lungs. This is rarer than a DVT but can be fatal.
You will be given blood-thinning medications to lower the risk of getting clots. The sooner you are walking and more active, the lower the risk of getting blood clots. Again, this is why I use enhanced recovery programs to enable my patients to be up and walking early.
It is advisable to not go on any long distance flights for at least six weeks, but it is better still if you delay for 12 weeks.
Nerve injury
Numbness in the front of the thigh can occur but it’s not a cause of pain. Rather patients are aware of an altered sensation. Very rarely, the nerve that supplies muscles to the ankle and foot (sciatic nerve) may get compressed or damaged leading to a foot drop.
Fracture
When placing the metal implants into the bone a crack or fracture can occur. If visible, I will fix the fracture there and then. Sometime the fracture is not visible until X-Rays are performed. Depending on the extent of the fracture, another operation may be required, but this is rare
Dislocation
The artificial ball can pop out of its socket as it is smaller than the native ball. If this should occur, then some form of sedation is required in hospital to relocate it. The greatest risk of dislocation is in the first 12 weeks after surgery. The dislocation rate for my patients is less than 1%.
Leg length discrepancy
Sometimes, the operated leg becomes slightly longer than the other. This is because the muscle needs to be tensioned in order to make the hip more stable and lower the risk of dislocation. We do this because it is a lot more problematic having a hip that pops out (dislocates) than one leg shorter than the other.
Stiffness and ongoing pain and swelling
It is imperative that you do exercises at home to regain the movement you had in your hip before the surgery or to improve it afterwards. The physiotherapist usually give you a program to do. Nonetheless, stiffness in the hip can still occur. This is usually dealt with extensive physiotherapy.
Dissatisfaction rate of 10%
All patients that have had joint replacement surgery in the UK have their data entered in the National Joint Registry. This is the largest registry of its kind in the world and has approximately 3 million entries. From this data, we can conclusively say that a hip replacement is a successful operation 90% of the time. However, this means that there is still a dissatisfaction rate of around 10%. A lot of research is going into why this is the case and I have presented in several international meetings regarding this.
Loosening
All artificial joints have a finite lifespan and wear out with time. The National joint registry has shown us that 90% of hip replacements last more than 15 years.
If you have any questions regarding this or any other hip or knee problems, give us a call. I will be very happy to help.
Complex total hip replacement in young patients
In some patients performing a total hip replacement can be more complicated due to abnormal anatomy. This is particularly so in younger patients who have hip dysplasia or DDH. This is because the socket may not be fully developed, or there may be areas of bone loss. Young patients with DDH may need a hip replacement much earlier (e.g. in the 20s or 30s). In addition, the shape of the thighbone may be abnormal further complicating the operation.
As a result of my fellowship training, and extensive consultant experience in dealing with young adults with hip problems, I have vast experience in reconstructing these complex joints. I use a variety of implants in the socket and the femur, thus allowing me to recreate the hip joint anatomically. I pay careful attention to restoring the leg length, which can be a problem in such patients and this ultimately leads to a better functioning hip joint. On occasions, I have used custom-made prostheses because the anatomy is so distorted. When there has been bone loss I have also had to use bone graft either from the patient or form a donor. When bone graft cannot be used I have used highly specialised metal, mimicking the character of the patient’s bone and integrating well with it. This is called Tantalum or Trabecular Metal.
If you’re suffering from pain and stiffness in your hip joint, the first step to feeling better is to schedule an appointment with Mr Parag K. Jaiswal, an expert in Young Adult Hip problems. I will be happy to discuss all treatment options, especially ones that can save your joint. To request an appointment call on (020) 7459 4482
Download your free guide on what questions to ask your orthopaedic Consultants here.
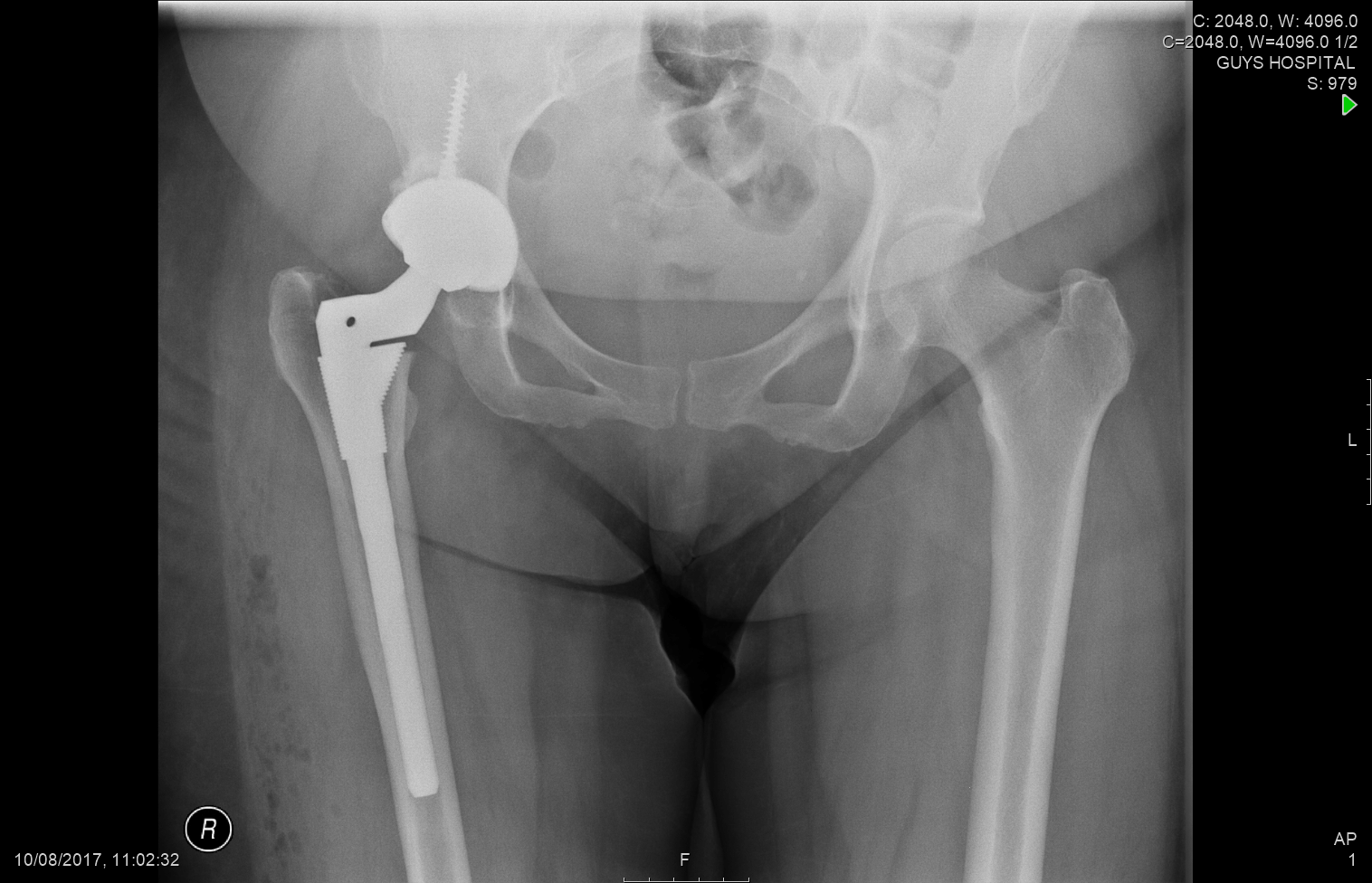
This is an X-Ray of a 36 year old female, Notice the difference in the shape of he socket and how on the left the socket is not completely covering the entire ball. There is severe joint space narrowing, the femoral bone almost touching the socket bone. The femur is significantly twisted (anteverted) which is nor readily appreciated on the X-Rays.
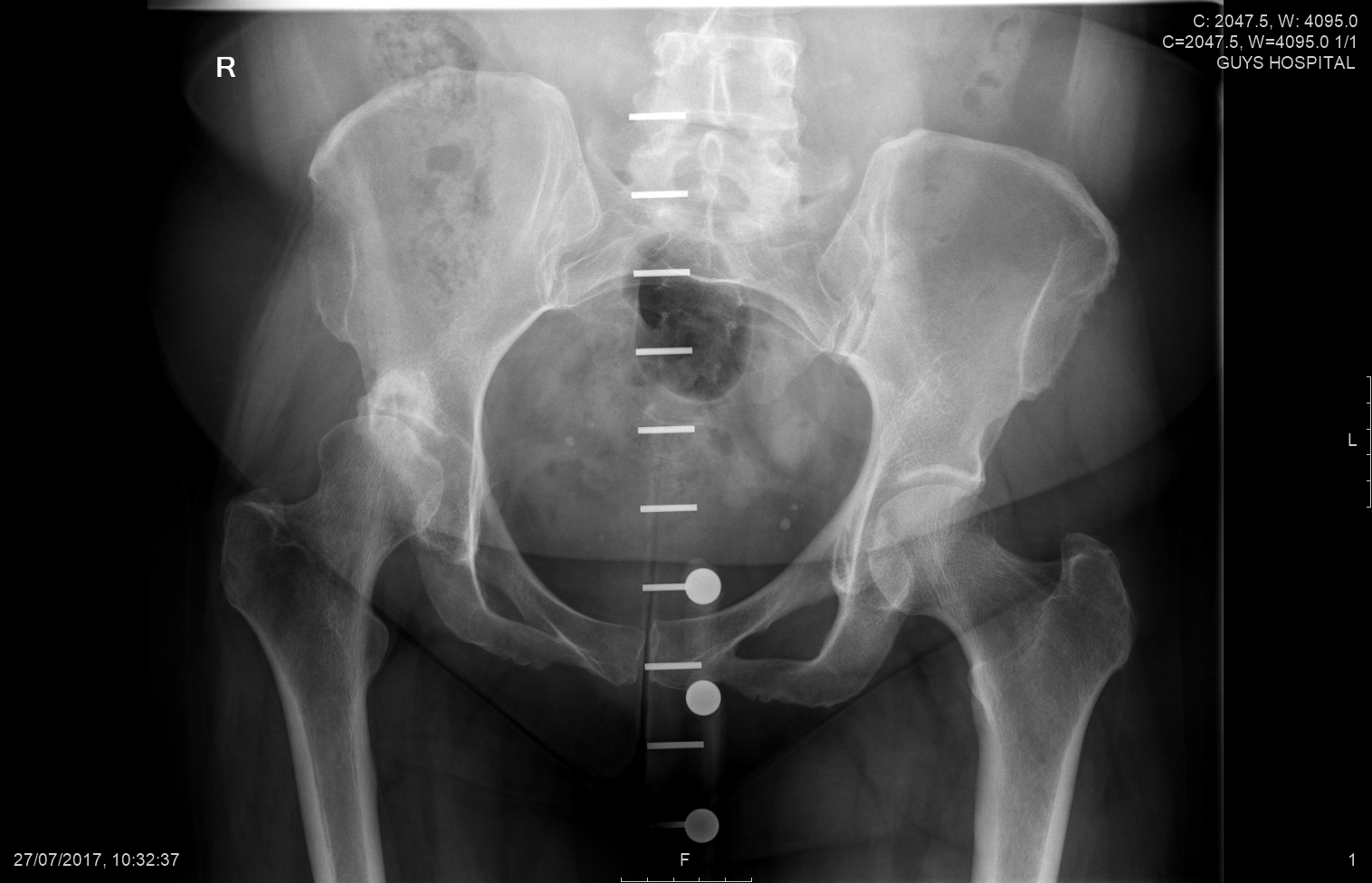
I used a special kind of cup which ‘grips’ the socket bone very well as there was some bone loss. This is a very specialised kind of implant in the thighbone which allows me to adjusts the amount of native twist in the this patients thigh bone (femur). The patient was able to go home after just 2 days as a result of the minimally invasive techniques and enhanced recovery programs I use.
Why choose Mr. Jaiswal?
I perform minimally invasive hip surgery and use enhanced recovery protocols to ensure patients have the least possible pain and fastest recovery following surgery. I have extensive international experience from Canada and USA, where I learnt cutting edge surgical techniques and use the best possible implants tailored to the patients’ needs. Above all, I am an empathic listener, and ensure that I answer all your questions and allay all your fears and concerns about the whole journey.
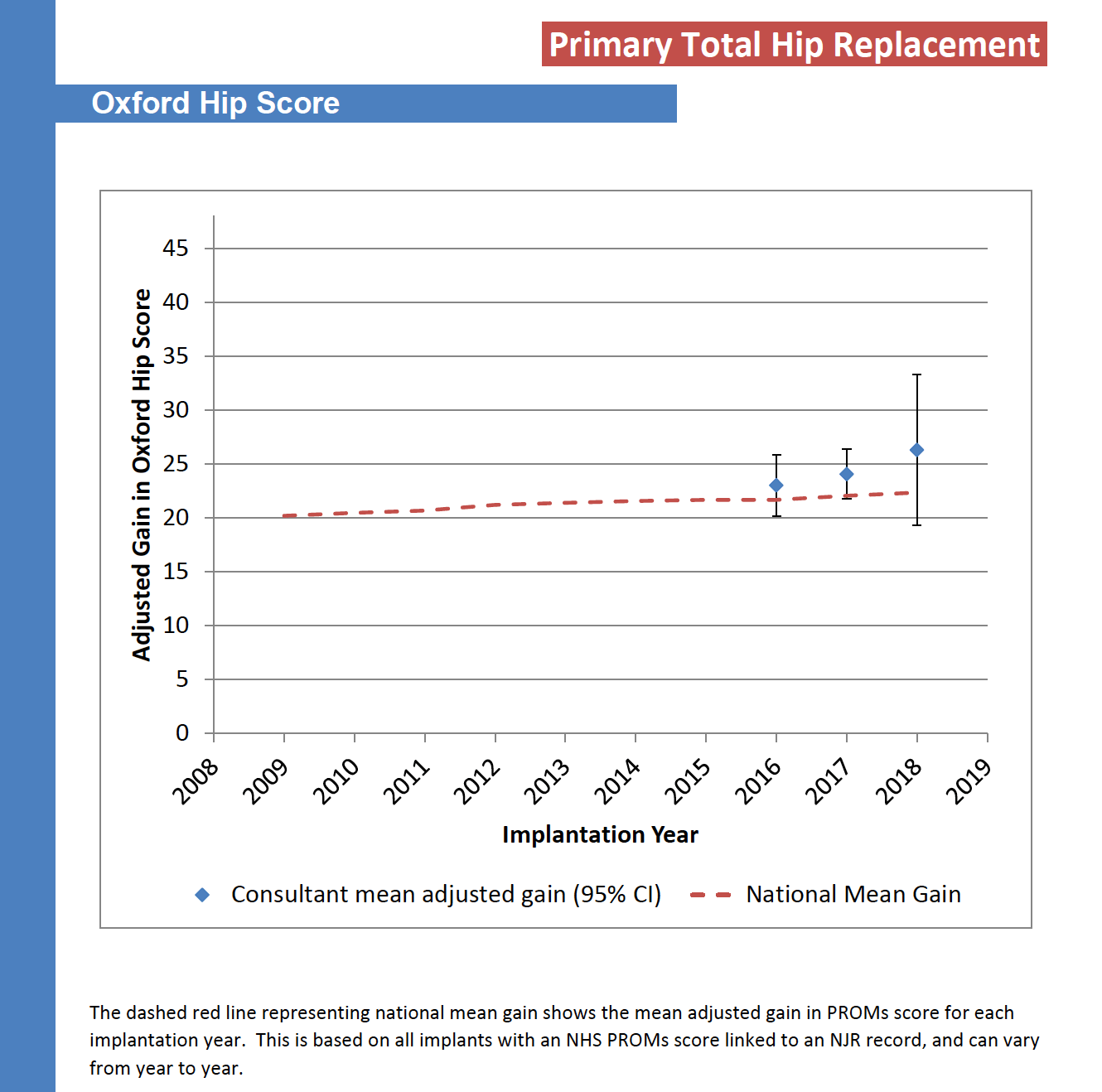
As I mentioned previously, all patients undergoing joint replacement surgery have their data entered in the National Joint Registry (NJR). All patients are requested to fill in a 12-point questionnaire assessing the pain and function in their hip (called the Oxford Hip Score) before and 6 months after surgery. The graph below shows that my patients (blue circle) have experienced greater gains than the national average (red dashed line) following a hip replacement and tend to do better.